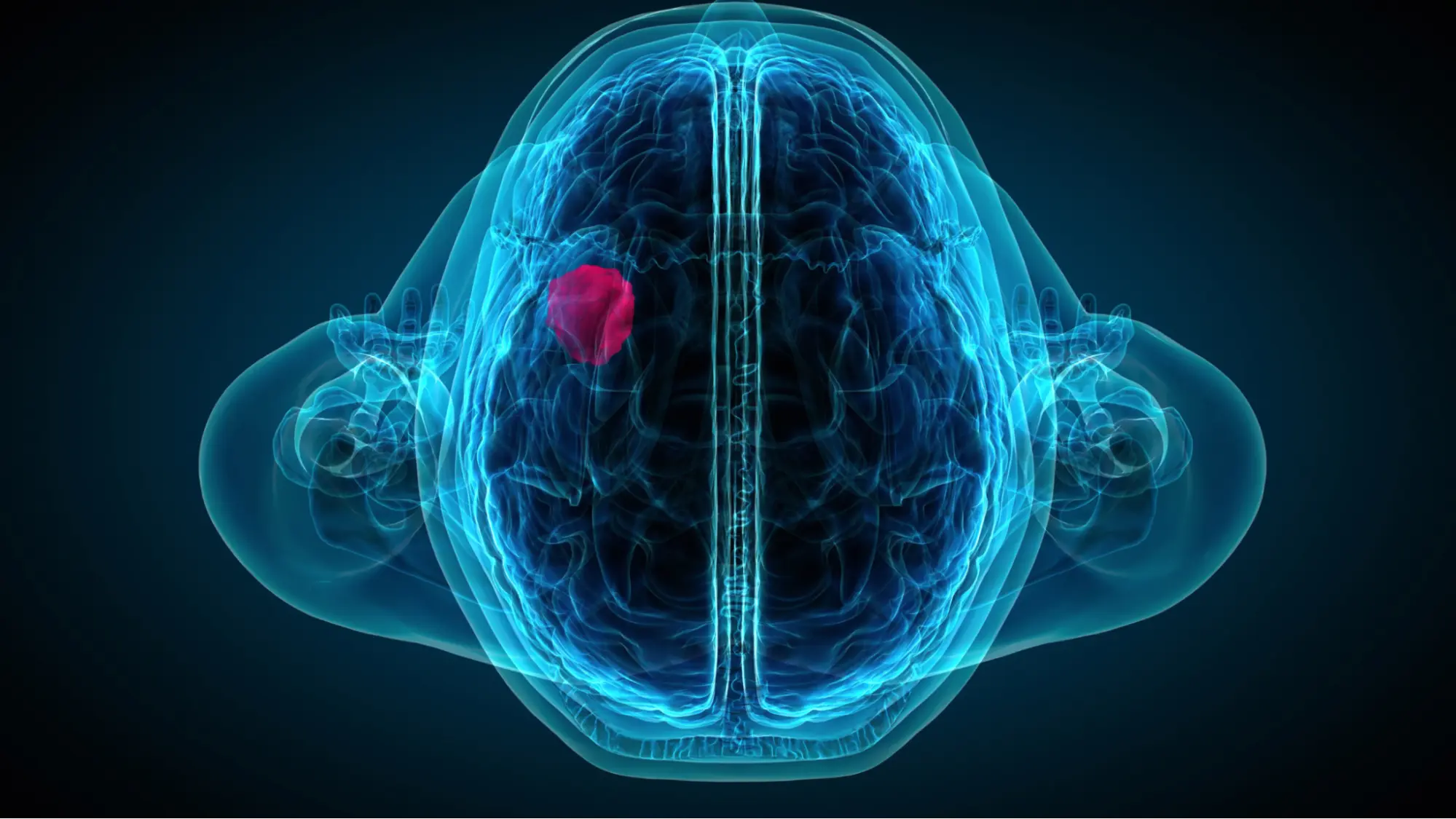
Brain tumors represent a heterogeneous group of pathologies that can originate in the brain itself (primary brain tumors) or be the result of metastasis of tumor lesions in other organs (secondary brain tumors). Although their incidence is relatively low compared to other types of cancer, their clinical impact is significant due to the anatomical and functional complexity of the central nervous system.
In recent decades, progress in neurosurgery has completely transformed the therapeutic approach to these cases. The combination of techniques such as neuronavigation, fluorescence-guided resection and awake surgery has made it possible not only to increase tumor resection rates, but also to preserve neurological function, even in tumors located in eloquent areas of the brain.
Today, many brain tumors that were previously considered inoperable can be safely and accurately addressed.
In this article we explore how technological advances are changing the natural history of this disease, making more effective and personalized treatments possible.
What is a brain tumor and how is it classified?
A brain tumor is an abnormal mass or growth of cells in the brain or its adjacent structures. They can be classified according to two main criteria:
According to their origin:
- Primary: These are lesions that originate in the brain tissue itself. E.g.: gliomas, ependymomas, etc.
- Secondary (metastatic): they come from tumors located in other parts of the body (lung, breast, melanoma…).
According to their behavior:
- Benign: slow growing, non-infiltrating, lower risk of recurrence after resection.
- Malignant: rapid growth, invasion of brain tissue, potential for recurrence or spread.
The World Health Organization (WHO) classifies central nervous system tumors from grade I to IV, with grade IV (glioblastoma multiforme) being the most aggressive.

What are the symptoms of a brain tumor?
Symptoms depend on the location of the tumor rather than its type. Some common signs include:
- Persistent headache, especially upon awakening.
- Vomiting without apparent cause.
- Seizures in patients without a history of epilepsy.
- Neurological alterations: loss of vision, weakness in a limb, language or memory difficulties.
- Personality or behavioral changes.
In many cases, symptoms appear progressively, which may delay diagnosis.
Diagnosis of brain tumors: key tools
The diagnostic process includes:
- Complete neurological examination.
- Advanced neuroimaging: High resolution magnetic resonance imaging (MRI) with contrast is the test of choice. It allows to assess size, location, mass effect, associated edema and uptake characteristics.
- Computed tomography (CT): useful in emergency situations.
- Biopsy: in selected cases, it is performed to confirm the histological type before starting treatment.
In some cases, functional resonance, tractography and spectroscopy are used, especially for planning surgery in eloquent areas.
Technological advances in the surgical treatment of brain tumors
Neuronavigation: millimetric precision
Neuronavigation acts as a surgical GPS. It allows the neurosurgeon to visualize in real time the exact position of the instruments inside the brain, guided by preoperative images (MRI or CT).
Advantages:
- More precise resections.
- Avoid critical structures.
- Less postoperative neurological damage.
It has become a standard in neurosurgical oncology.
Fluorescence-guided resection
It consists of the preoperative administration of substances such as 5-ALA (5-aminolevulinic acid), which is selectively metabolized in tumor cells. Under blue light in the operating room, the tumor glows with fluorescence, facilitating its differentiation from healthy tissue.
Main applications:
- High grade gliomas.
- Increases the rate of complete resection.
- Improved progression-free survival.
Studies such as that of Stummer et al. (Lancet) demonstrate that fluorescence-guided resection improves surgical outcomes in glioblastoma.
Awake craniotomy surgery (awake craniotomy)
Indicated in tumors located in eloquent areas (language, motor), this technique allows the neurosurgeon to monitor functions in real time while removing the tumor.
The patient is conscious (sedated, pain-free) and performs guided tasks: talking, moving a limb, counting….
Benefits:
- Allows wider resections in critical areas.
- Minimizes the risk of neurological sequelae.
- Improves postoperative quality of life.
This technique requires a specialized and multidisciplinary team, specific training and careful patient selection.
Is it possible to completely remove a brain tumor?
It depends on the type, location and degree of infiltration.
- Benign encapsulated tumors (colloid cysts, pilocytic astrocytomas): high probability of complete resection.
- Low grade or diffuse gliomas: they can be partially resected and monitored over time.
- Glioblastomas or other infiltrating tumors: they can rarely be 100% removed, but extensive resection improves the prognosis and allows adjuvant treatments such as radiotherapy or chemotherapy to be more effective.
What other techniques support surgery?
- Intraoperative 3D ultrasound: allows the tumor to be visualized in real time during surgery.
- Intraoperative MRI (iMRI): updates brain images during surgery.
- Intraoperative electrophysiology: monitors motor or sensory function during resection.
- Microsurgery: the latest generation surgical microscope (with fluorescence) is the neurosurgeon’s essential tool when removing a brain tumor.
What happens after surgery? Rehabilitation and follow-up
The immediate postoperative period is monitored in the ICU or Neurosurgery Unit. From there, it is planned:
- Early neurological rehabilitation (physiotherapy, speech therapy, occupational therapy).
- Oncology follow-up with neuro-oncology and radiotherapy.
- Periodic imaging controls (MRI every 3 to 6 months, depending on the type of tumor).
The multidisciplinary approach is essential to maintain the patient’s quality of life.
What is the prognosis of a patient with a brain tumor?
The prognosis varies according to:
- Histological grade of the tumor (according to WHO).
- Age and general condition of the patient.
- Degree of resection achieved.
In general:
- Benign tumors have a very good prognosis after surgery.
- Low grade gliomas can remain stable for years with surveillance.
- Glioblastomas require multimodal treatment, with median survival of 12-18 months, but each case is unique.
The key is early diagnosis + specialized equipment + advanced surgical technology.

A new era in oncologic neurosurgery
Having a brain tumor no longer means what it did 20 years ago. Today, thanks to technology, many patients can benefit from safer, less invasive interventions with better functional outcomes.
The combination of clinical expertise and technological resources has broadened the horizons of what is possible. It is not just a matter of removing a tumor: it is a matter of doing so without sacrificing function, autonomy and the patient’s life.
If you have been diagnosed with a brain tumor or know someone in that situation, the most important thing is to put yourself in the hands of a specialized team that has all these resources.
📍 Dr. Andrés Muñoz – Specialist in Neurosurgery and Spine Surgery
📞 609 688 469
www.drandresmunoz.com
👉 Request your consultation here



