If you are facing your first spine surgery, you may be concerned about the amount of information and questions about the procedure. As a neurosurgeon specializing in spine surgeryI have had the opportunity to help many patients prepare for this procedure, and I know how important it is to understand every step of the process.
A correct physical and mental preparation not only improves surgical results, but also reduces risks and speeds up recovery. Therefore, in this article I will explain in detail everything you need to know, without unnecessary technicalities.
The importance of proper preparation for spine surgery
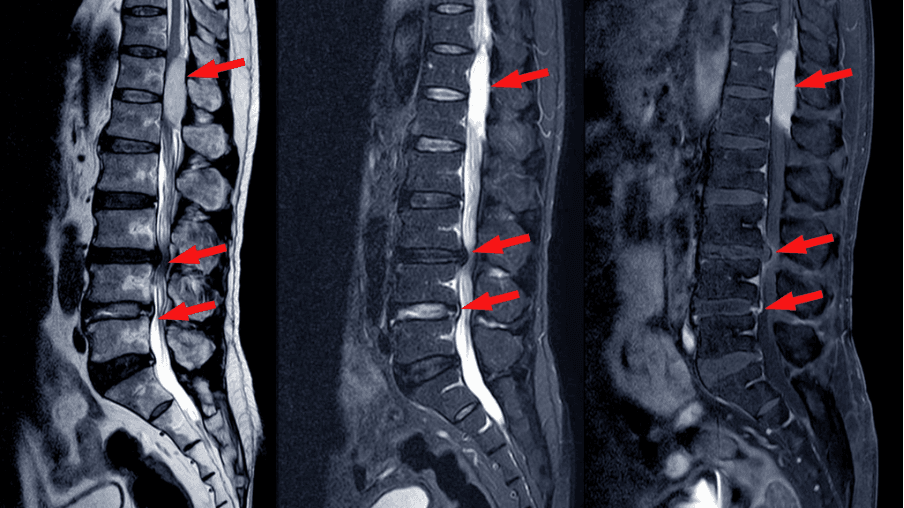
The spine is made up of 33 vertebrae distributed in five regions (cervical, thoracic, lumbar, sacral and coccygeal), which are interspersed with intervertebral discs that act as shock absorbers, absorbing impacts and allowing some mobility between vertebrae. This structure, together with ligaments, tendons and muscles, has key functions:
- Body support and balanceThe spine supports the weight of the head, torso and limbs. Thanks to its flexible and resistant structure, it allows to maintain an upright posture and to distribute the weight in a balanced way.
- MobilityAlthough at first glance it may appear rigid, the spine allows a great variety of movements: flexion, extension, rotation and lateroflexion. These functions are controlled by the facet joints, located at the back of each vertebra.
- Protection of the central nervous systemSpinal cord: The spinal canal houses and protects the spinal cord, which is the main conduit of communication between the brain and the rest of the body. Spinal nerves emerge from each segment of the cord and are responsible for sending and receiving motor and sensory signals. Injury or compression of the cord or these nerve roots can cause neurological deficits.
Spinal problems can cause chronic pain, loss of mobility or even neurological complications such as limb weakness. When these pathologies do not resolve with conservative treatments, surgical intervention may be necessary. Although its goal is to correct the cause of the problem – for example, to eliminate a nerve compression or stabilize a vertebra – the success of the operation depends on multiple factors, including the patient’s general condition and preoperative preparation.
Data supporting the preparation of the column operation
Clinical studies have shown that good preoperative preparation significantly improves surgical outcomes and reduces the risk of complications. Factors influencing the success of surgery include:
- General physical condition: the paravertebral musculature, i.e. the back muscles, play a fundamental role in the stability of the spine. It is necessary to maintain a certain degree of physical activity, even if the patient is in pain, prior to spinal surgery.
- Control of pre-existing diseases: conditions such as diabetes, hypertension or obesity can increase the risk of infections or scarring problems. It is essential that these conditions are controlled prior to surgery.
- Psychological preparation: studies have shown that patients with high levels of preoperative anxiety tend to report greater pain perception postoperatively. Although not a direct medical factor, managing stress through proper patient-physician communication can improve the overall experience of the procedure.
- Healthy habits: quitting smoking before surgery is crucial. Relevant data, presented at the 2013 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS), shows that the risk of pseudarthrosis (when bones do not fuse properly) is 2.3 times higher in smokers. In addition, the mean healing time for fractures is significantly longer in smokers (25.1 weeks) versus non-smokers (23 weeks).

Understanding spine surgery
Spine surgery has evolved significantly in recent decades. Thanks to technological and surgical advances, it is now possible to perform interventions with minimally invasive techniques. These techniques have revolutionized the treatment of different spinal pathologies by reducing surgical trauma, shortening recovery times and improving functional results.
The goal of any spine surgery, whether traditional or minimally invasive, is to correct structural or neurological alterations, such as herniated discs, canal stenosis or vertebral fractures, that affect stability, neurological control or spinal function. However, the minimally invasive approach is gaining more and more relevance, especially in cases where open surgery could pose greater risks.
What is minimally invasive spine surgery (MISS)?
Minimally invasive spine surgery is based on the use of small incisions, often smaller than 2-3 cm, and the application of specialized tools such as surgical microscopes, endoscopes and/or tubular spreaders. Unlike conventional surgery, which requires a wide opening of muscle tissue, MISS preserves much of the muscle and ligament structures, reducing damage to surrounding tissues.
The main advantages of this technique include:
1. Less postoperative pain: by avoiding large incisions in the tissues, pain after the operation is significantly less.
Reduced hospital stay: in many cases, patients can be discharged the same day or after a short hospital stay of 24 to 48 hours.
3. Faster recovery: functional recovery is usually faster, allowing patients to return to their daily activities and work sooner.
4. Lower risk of infection and complications: being less invasive, the possibility of infections and surgical complications is lower compared to open surgery.
Indications for minimally invasive spine surgery
Although MISS is not indicated for all cases, it is frequently used to treat various vertebral pathologies, such as:
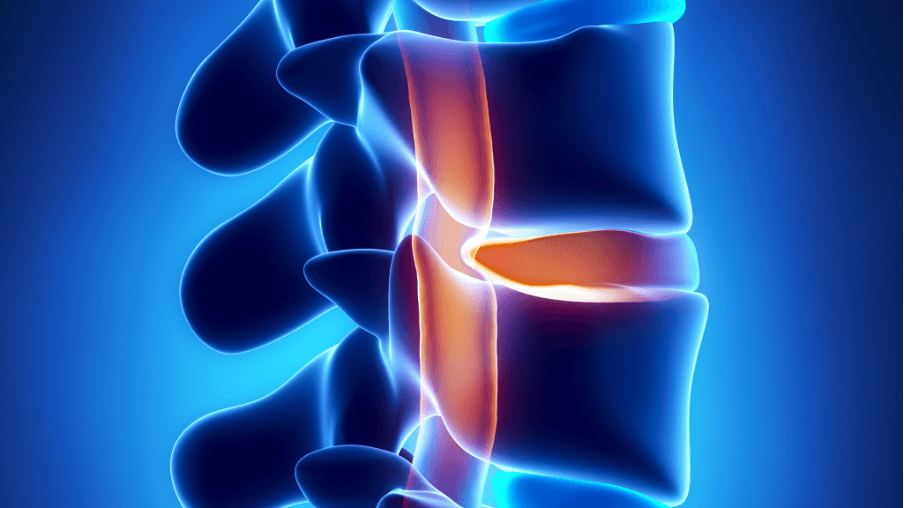
Herniated disc
In a minimally invasive microdiscectomy, through a small incision and with the aid of a surgical microscope, access is gained to the affected disc space to remove only the portion of the herniated disc that is compressing the nerve root, preserving the rest of the disc.
This technique provides effective symptom relief with minimal damage to the paravertebral muscles, which significantly improves the postoperative period.
2. Canal stenosis
In decompressive laminectomy, the surgeon removes the bony structures and/or tissues compressing the nerve structures, also by microsurgical technique, which allows maintaining the functional integrity of the muscles.
3. Arthrodesis (spinal fusion)
Percutaneous arthrodesis is used in cases of spondylolisthesis (vertebral displacement) or vertebral fractures associated with instability. In this procedure, pedicle screws are inserted through small incisions, guided by intraoperative imaging techniques such as fluoroscopy or surgical navigation. Subsequently, rods are placed to stabilize the affected vertebrae. This approach reduces the risk of excessive bleeding and minimizes hospital stay.
4. Vertebroplasty (vertebral cementation)
Vertebroplasty is another percutaneous technique that is usually used in fractures with vertebral subsidence, generally of an osteoporotic nature, which are not associated with instability. It consists of introducing a substance (methylmethacrylate) through a small trocar inside the vertebral body to try to consolidate the vertebra and secondarily, to reduce pain by reducing the inflammatory tissue inside the vertebra.
When is surgery necessary?
Spine surgery is recommended when symptoms do not improve with conservative treatments, such as physiotherapy, anti-inflammatory drugs or infiltrations. Among the factors that determine the surgical indication are:
1. Significant nerve compression: If a herniated disc or spinal stenosis causes severe pressure on the nerves, symptoms such as weakness or loss of sensation may occur.
Mechanical instability: some conditions, such as spondylolisthesis (displacement of a vertebra), generate abnormal movements between the vertebrae, causing pain and dysfunction. In these cases, stabilization surgery may be necessary.
2. Preoperative physical preparation
Medical evaluations required prior to spine surgery
Before any surgery, it is essential to perform a series of preoperative tests to evaluate your overall health. These tests include:
- Blood tests: to detect coagulation problems or anemia.
- Cardiovascular evaluation: it determines, by means of an electrocardiographic study, the existence of any type of cardiac rhythm disorder (arrhythmias) that may pose a risk during the intervention.
These tests help to identify possible risk factors and to plan the procedure in a safer way.
Recommended routines to improve the supporting musculature
The paravertebral musculature (the muscles that surround and support the spine) plays a critical role in spinal stability. It may be advisable to perform controlled exercises, such as gentle stretching or isometric strengthening work, can help improve your condition prior to surgery. A well-conditioned back recovers more quickly after surgery.
Nutrition and healthy habits before surgery
Tissue healing requires a good availability of nutrients. Make sure you consume enough protein, which is essential for cell regeneration, as well as foods rich in vitamin C (which promotes collagen production) and vitamin D (which improves bone health).
If you are a smoker, I advise you to stop smoking before surgery, as it decreases the ability to heal and increases the risk of infection.

3. Emotional preparation from the clinical approach
Reducing uncertainty through accurate information
It is normal for fear of the unknown to generate anxiety. Many patients are relieved when they understand what will be done during surgery, what the recovery will be like and what the risks are. During preoperative consultations, I strive to explain these details clearly, because a well-informed patient approaches the operation with greater peace of mind.
Effective communication with the medical team
Trust your medical team. If you have questions, don’t hesitate to ask them. Being in tune with your neurosurgeon and healthcare staff is key to approaching this process with confidence.
4. The day of surgery: planning and procedures
Pre-operative instructions
You may be asked to fast for 6 to 8 hours before the procedure. You will also need to avoid certain medications, such as anticoagulants or antiplatelet drugs, which may increase the risk of bleeding. Upon arrival at the hospital, you will undergo basic check-ups and be prepared for the operating room.
What to expect in the operating room
The procedure will be performed by a specialized medical team. You will be under anesthesia, which means you will not feel pain. Depending on the type of surgery, the procedure may last between 1 and 4 hours. After the operation, you will be transferred to a recovery room to monitor your vital signs.
5. Postoperative recovery
Hospital care
Pain control is a priority in the first few hours, so you will be given painkillers as needed. Your ability to move around will also be evaluated and, in some cases, you will begin to walk around a few hours after the procedure. Discharge from the hospital usually takes place 24 hours after the procedure.
Home care and warning signs
Upon discharge, you will receive instructions on how to care for the surgical wound, what activities to avoid and when to come in for check-ups. Pay attention to symptoms such as fever, excessive swelling or discharge from the wound, as these may indicate a complication.

6. Long-term rehabilitation and prevention
Importance of physiotherapy
Once the tissue has healed, physical therapy can be very helpful in regaining strength and mobility. A physical therapist will guide you through specific exercises designed to prevent stiffness and improve spinal function.
Relapse prevention
Adopting healthy habits, such as maintaining good posture, avoiding carrying excessive weights and exercising regularly, is key to preventing future injuries.
Spine surgery can significantly improve your quality of life if you prepare properly. As a neurosurgeon, my mission is to ensure that every step of this process is performed safely and with as little risk as possible. Follow your doctor’s instructions: you’ll be on the road to a successful recovery.
Do you need an evaluation for spine surgery? In my offices in Cadiz, Malaga, Seville and Huelva we will evaluate your case and guide you to the most appropriate treatment.
Frequently asked questions about spine surgery
Why is good preparation for spine surgery important?
Minimally invasive surgery reduces surgical trauma, shortens recovery times and improves functional outcomes. It offers less postoperative pain and reduces hospital stay.
Why is it important to have a good physical preparation before spine surgery?
Good physical condition improves surgical results and reduces risks. This includes maintaining good paravertebral musculature and performing gentle exercises before surgery.
When is spine surgery necessary?
Surgery is recommended when symptoms do not improve with conservative treatments, such as in cases of significant nerve compression or mechanical instability.
What medical tests are necessary before spine surgery?
Blood tests and cardiovascular evaluations are required to detect coagulation problems or heart rhythm disorders.
Why is it important to stop smoking before spine surgery?
Smoking increases the risk of complications and delays healing. The risk of pseudarthrosis is higher in smokers.
How can I prepare myself emotionally for spine surgery?
Clear communication with the medical team and accurate information about the procedure can reduce anxiety.
What care is necessary during recovery at home after spine surgery?
Control pain, care for the surgical wound and avoid activities that may cause complications. Pay attention to symptoms such as fever or excessive swelling.
What is the role of physical therapy in recovery after spine surgery?
Physiotherapy helps to recover strength and mobility, preventing stiffness and improving the functionality of the spine.
How can I prevent future spinal injuries after surgery?
Maintain good posture, avoid carrying excessive weights and exercise regularly.
When is it necessary to seek a second opinion on spine surgery?
If you have doubts about the diagnosis or the recommended treatment.



