Imagine getting up every day without that back pain that limits you at every step, without the fear of making a wrong move that makes things worse. Does it sound like a dream? The spinal neurosurgery could be the key to achieving that quality of life you so desire, but the very idea of surgery brings understandable fears. The spine is a delicate anatomical region and it is normal that a surgical approach can generate anxiety.
However, most of these fears are based on myths. Today, the neurosurgery of the spine has advanced enormously, and minimally invasive minimally invasive techniques that make the surgery safer, faster and with a much quicker recovery, with a lower rate of complications. In this article I will explain to you what is really a spinal neurosurgeryThe following are some of the reasons why the fear of undergoing surgery should not hinder your quality of life.
Spinal neurosurgery: what is it and when is it recommended?
The spinal neurosurgery is an intervention aimed at relieving pain or physical limitations resulting from structural problems in the spine, such as: hernias, osteoporotic fractures, stenosis (narrowing of the spinal canal).
This procedure is based on a series of minimally invasive surgical techniques. minimally invasive surgery, performed by a neurosurgeon neurosurgeon who must perform a complete evaluation to determine the diagnosis and whether surgery is the best option, considering the evolution of each case and the impact of other non-invasive treatments.
The spinal neurosurgery is indicated when conservative treatments, such as physiotherapy, medication or pain unit techniques, have not been sufficient to improve the symptomatology. Surgery then becomes an opportunity to give back to the patient the quality of life that has been lost due to pain or the important physical limitations derived from this situation.

Most common diseases of the spine
Herniated discs
The herniated discs are one of the most common causes of spinal surgery. They occur when the intervertebral disc, which acts as a shock absorber between the vertebrae, becomes displaced or ruptures, causing the inner nucleus of the disc to press on an adjacent nerve. This nerve compression can cause intense and debilitating pain, as well as radiating into the extremities (brachialgia or sciatica), producing symptoms such as numbness and loss of strength in the extremities. The most commonly used procedure in neurosurgery is the microdiscectomywhich consists of removing the herniated disc fragment and freeing the compressed root.
Spinal canal stenosis
The spinal stenosis occurs when the spinal canal narrows and puts pressure on the spinal cord or nerve roots. This condition is common in older people, as wear and tear on the discs and joints can lead to progressive narrowing of the spinal canal. Symptoms include back pain, numbness, and weakness in the legs or arms, which can make mobility difficult ( claudication) and affect daily activities.
The surgery is an option in severe cases of stenosis, especially when there is a risk of permanent nerve damage or when pain severely limits physical activity. Procedures such as laminectomy and foraminotomy, with microsurgical technique, allow decompressing the spinal canal, eliminating small portions of bone and tissues that are obstructing the passage of the spinal cord and nerves. These procedures aim to widen the spinal canal, relieving symptoms and restoring quality of life.
Vertebral fractures
The vertebral fractures usually occur as a result of trauma, accidents or, more commonly, in degenerative bone diseases such as osteoporosis. osteoporosis. These fractures produce inflammatory pain and can compromise spinal stability. In severe cases they can put the spinal cord and nerves at risk, making surgery a necessary option to avoid irreversible damage. In selected cases, a minimally invasive, percutaneous intervention such as the vertebroplasty (vertebral cementation) can stabilize vertebral subsidence and significantly reduce inflammatory pain.
Common myths about spine surgery that increase fear
The fear of spinal surgery is linked to several myths that, unfortunately, many people continue to believe as:
Myth 1: “Spine surgery is painful and recovery is complicated”.
RealityIn the past, spine surgeries were more invasive, requiring large incisions and a lengthy recovery process. Today, there are minimally invasive techniques, such as microdiscectomy or vertebroplastysuch as microdiscectomy or vertebroplasty, which require only small incisions, minimize postoperative pain and allow the patient to return to normal life in much less time.
In a microdiscectomy, for example, a small incision is made and a microscope is used to remove the part of the disc that is affecting the nerve. This technique reduces trauma to the surrounding tissues, which means a faster and less painful recovery. The patient may be able to return to normal activity within a few weeks.
Myth 2: “Spinal surgery always involves a risk of paralysis or spinal cord involvement.”
RealityAlthough all surgery has risks, the probability of paralysis in spinal surgery is extremely low. In fact, in lumbar spine surgery, a spinal cord injury cannot occur, since the spinal cord does not reach the lumbar area (it ends at the level of the last dorsal vertebra); therefore, the famous phrase of: “will I stay in a wheelchair?” not applicable, when we talk about lumbar spine surgery.
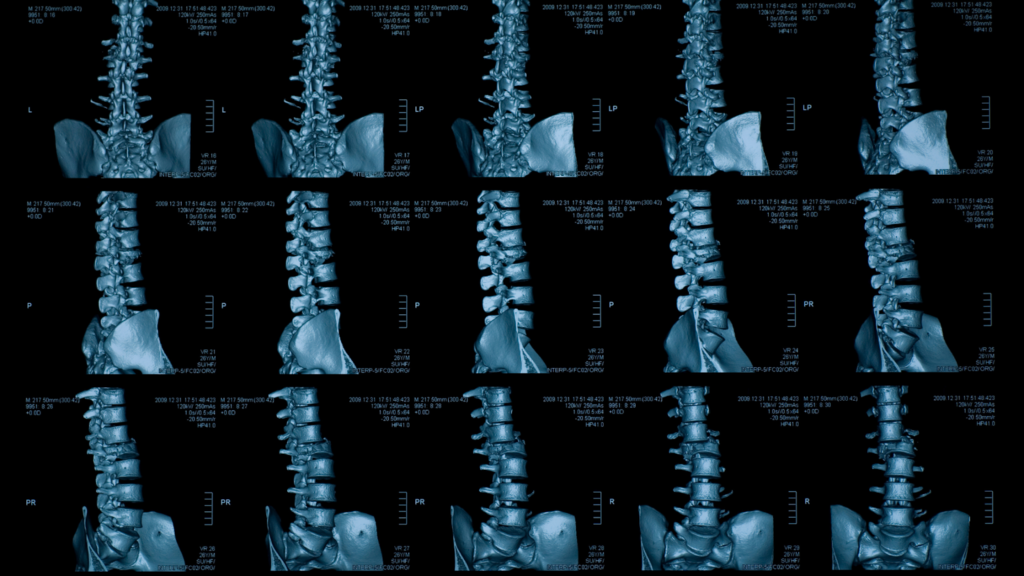
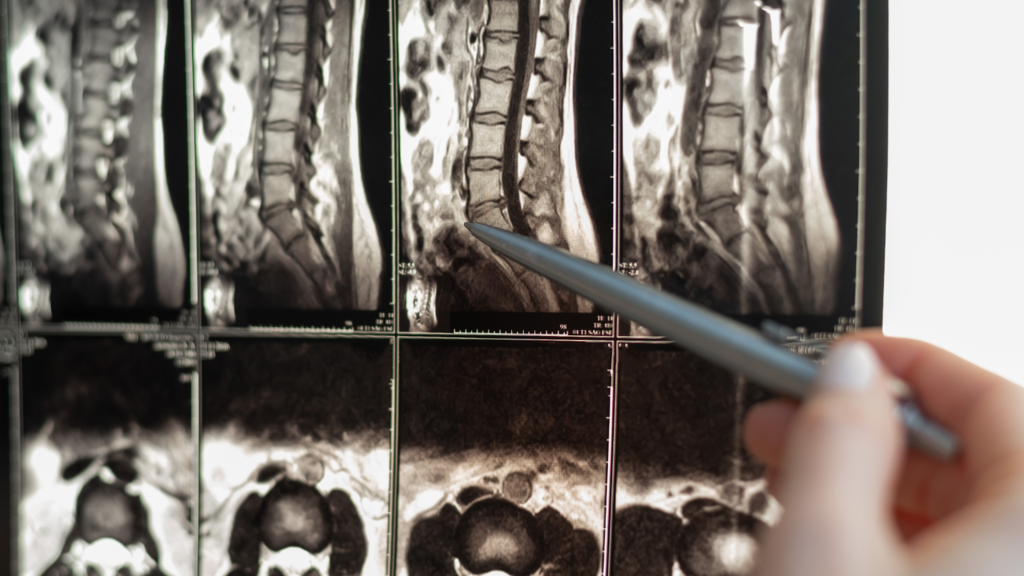
Today, the use of navigation techniques navigation techniques y microsurgery allows the neurosurgeon to operate with greater precision, avoiding critical areas of the spinal canal. In addition, each surgery is meticulously planned through magnetic resonance imaging, which allows the structures to be clearly identified before operating.
Myth 3: “Will I need plates and screws if I have spinal surgery?”
RealityNeurosurgeons are generally more microsurgical and offer nerve decompression (which is, after all, the origin of the painful symptom) without the need to instrument the spine.
How do we achieve this? Well, by trying to remove as little bone as possible to access the inside of the canal; once inside, with microsurgical technique the ligament is released (in case of stenosis) or the disc fragment (in case of herniation) until an adequate radicular decompression is achieved. If we remove too much bone to perform the decompression, long-term instability could be generated, which is why some specialists decide to instrument the spine during the operation, but this is not our case.
Myth 4: “The results of spine surgery are not long lasting”.
RealitySpine surgery: Advances in surgical techniques have led to long-lasting results in spine surgery. Most patients experience significant relief after surgery. However, it is important to understand that, as with any treatment, the success of surgery also depends on postoperative follow-up and the patient’s lifestyle habits.
It is essential that, after surgery, patients follow medical recommendations, perform physiotherapy exercises and maintain an active and healthy lifestyle to maintain the results. Surgery is only part of the process; self-care is the key to enjoying a better quality of life in the long term.

What should I know before and after spine surgery?
Spine surgery requires a careful and detailed approach, both before and after the procedure. Below, I explain the most important aspects to keep in mind in order to prepare and recover properly.
Before surgery
- Consultation with a specialized neurosurgeon: it is essential that you go to a neurosurgeon with experience in spine surgery, since this specialist will guide you through every step of the process and will resolve all your doubts.
- Preoperative testsThe neurosurgeon may request imaging tests such as MRI scans, scans or functional studies such as electromyography to know the exact state of your spine and plan the surgery accurately.
- Emotional and mental preparationFeeling nervous is normal. Talking openly with your neurosurgeon and clarifying all your doubts will help reduce anxiety and give you a better perspective of the process.
After surgery
The success of the surgery also depends on a good postoperative period. Some key aspects of recovery include:
- Controlled restDuring the first days, it is advisable to make a relative rest. It is recommended to take walks, increasing the frequency and duration of these as the days go by.
- PhysiotherapyRehabilitation treatment is important to restore mobility and strengthen the paravertebral musculature. Following the neurosurgeon’s indications, it can generally be useful from the third week after surgery.
- Avoid exertionDuring the first weeks, avoid heavy lifting or activities that require intense physical exertion.
- Medical follow-upPeriodic check-ups with your neurosurgeon are key to evaluate recovery and prevent possible complications. We usually check the patient in consultation in the third week after surgery, once the stitches have been removed and before starting physiotherapy treatment.

Spine surgery: a step towards a better quality of life
The fear of spinal surgery is understandable, but it is also important to remember that, in many cases, the risk of not having surgery may be greater than the risk of the surgery itself. A well-planned operation performed by a neurosurgeon can not only relieve pain, but also significantly improve your quality of life.
One of the most important advances in spine neurosurgery spinal neurosurgery is the minimally invasive surgeryan approach that has completely changed the way in which surgical interventions are performed. Unlike traditional surgery, which requires extensive incisions to access the spine, instrumentation, etc., minimally invasive surgical techniques use small incisions, specialized instruments and advanced technology to perform the procedure with minimal trauma to the patient.
Benefits of minimally invasive spine surgery
The minimally invasive techniques in neurosurgery have brought about a true revolution in the treatment of spinal problems. Thanks to these innovations, it is now possible to perform procedures safely and efficiently, achieving a number of key benefits:
- Less trauma to the body: by avoiding large incisions and working with precision, tissue trauma is considerably less compared to open surgery. This means less postoperative pain and a more comfortable recovery for the patient.
- Faster recovery: Due to less muscle and tissue damage, recovery time is significantly shorter. In many cases, patients can resume their daily activities within weeks, instead of the months traditionally needed to recover from open spine surgery.
- Risk reduction: small incisions and precision instrumentation minimize the risk of infection and postoperative complications. In addition, visualization techniques allow the surgeon to avoid delicate areas of the spinal cord and nerves, making the procedure safer.
- Small scarsSmall incisions result in much less visible scars, which also contributes to an improved patient experience.
If you have been given a diagnosis related to a spinal problem, are considering this intervention or have any questions about the process, I will be happy to answer all your questions in my office or by contacting me via phone, social networks or our website.
Dr. Andrés Muñoz Núñez
Neurosurgeon
Málaga, Cádiz, Sevilla, Huelva
Phone: 951 749 631 / 609 688 469
Mail: neurocirugia@andresmunoz.es
www.drandresmunoz.com